Electronic Health Record vs Ippocra: Which One to Choose?
 Ippocra vs Electronic Health Record (EHR): Which One to Choose for Your Medical Reports
Ippocra vs Electronic Health Record (EHR): Which One to Choose for Your Medical Reports
Comparison between Ippocra and EHR, discover how to integrate them for complete control of your health documentation.
Have you ever tried to access your Electronic Health Record (EHR) the night before an important appointment, only to discover that the test you were looking for hadn’t been uploaded? Or worse: that you had to navigate different interfaces for each region where you had undergone examinations?
The promise of the EHR was clear: a single point of access for all your health documentation. The reality, for many patients, is quite different. And when it comes to your own health, relying on fragmented systems is not an acceptable option.
Guglielmo’s Case: When the EHR Isn’t Enough
“I’m on therapy for a chronic condition and I need to have the latest exams always at hand. The problem? Half of my medical reports are in Lombardy’s EHR, others in Lazio’s where I see a specialist, and some I only have as PDFs scattered across emails and WhatsApp. When my doctor asked for the complete history of the last two years, it took me three days to gather everything. It’s not sustainable.”*
— Guglielmo, 42, patient with a chronic disease
Guglielmo’s case is not isolated. It represents a daily reality for millions of Italians who have to manage their health through fragmented, bureaucratic systems, often inaccessible at moments of real need.
The Root of the Problem: Structural Fragmentation
The Electronic Health Record was created with a noble intent: to centralize citizens’ health documentation in a public system. However, practical implementation presents significant limitations:
-
Regional fragmentation: Each Italian region manages its own EHR with different platforms, upload standards, and non‑uniform timelines. A patient moving between regions must access different systems, each with separate credentials and interfaces.
-
Unreliable uploading: Not all health entities regularly upload medical reports to the EHR. Private labs, specialist offices, and some accredited facilities often operate outside the circuit, creating gaps in the patient’s documentation.
-
Difficulty finding documents: Every EHR is different per region. Some are more advanced than others, but searching for documents is always extremely complicated.
-
No images: Images cannot be uploaded to the EHR. It does not store X‑rays, CT scans, ultrasounds or large DICOM files.
These limits highlight the need for a complementary approach to the EHR that gives patients true ownership of their health documentation.
The Personal Centralization Method
The solution is not to abandon the EHR, but to pair it with a personal management system that fills structural gaps and returns control of documentation to the patient.
Ippocra takes a different approach: instead of replacing public systems, it creates a layer of personal ownership that integrates, organizes, and truly makes accessible the entire clinical history of the patient and their family members.
Smart Acquisition and Total Centralization
Unlike the EHR, which depends on uploads from health facilities, a personal management platform allows the patient to actively acquire their own medical reports from any source:
-
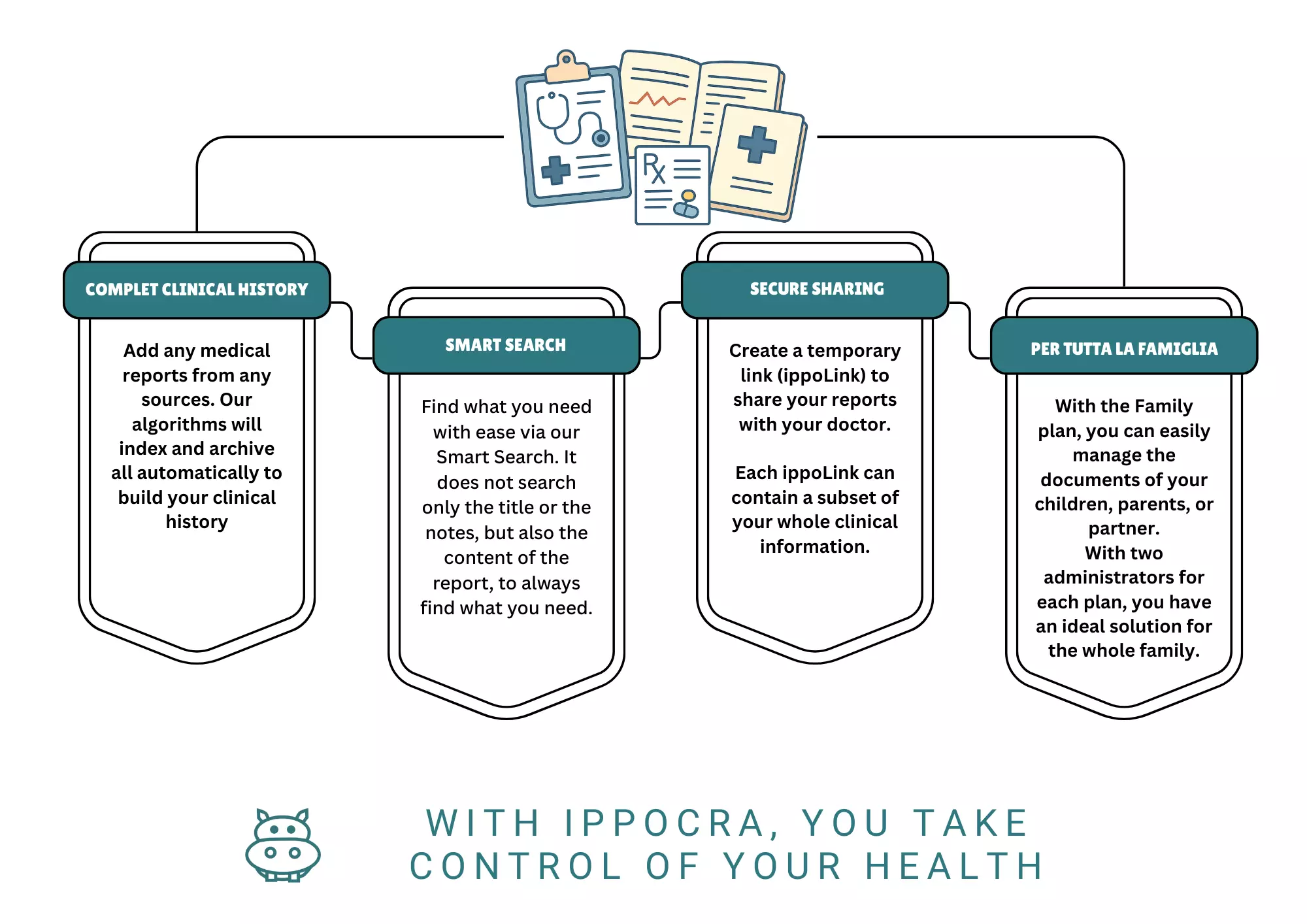
Complete clinical history with multi‑source integration: Ippocra lets you centralize all documentation. Emails from the analysis lab, PDFs downloaded from the hospital portal, documents received via WhatsApp from a specialist – everything converges into a single personal archive, without relying on institutional interoperability standards. This includes clinical records from private specialist visits, reports from various health facilities, and even photos of old paper documents.
-
User‑driven organization: Ippocra lets you organize documents however you wish. Our technology runs on genetic algorithms, automatically extracting clinical data from paper documents and converting them into a structured digital format. A report photographed from a private lab instantly becomes part of the clinical timeline.
-
Family‑wide clinical history: Ippocra is specifically designed to manage the clinical records of multiple family members. Users can collect and organize health information of children, parents, or partners within a single account, avoiding the need to juggle separate accesses or physical folders for each person.
-
More than documents: Ippocra also allows you to upload your CT scan or MRI to the platform, not just the radiology report.
Immediate Availability and Chronological Organization
The value of a health archive lies not only in its completeness, but in the ability to retrieve the right information at the right time:
-
Semantic search: Instead of navigating folders and dates, the patient searches by exam type, medical specialty, or time period. “All thyroid tests from the last two years” becomes an instant query, not a manual exploration.
-
Integrated clinical timeline: Medical reports are automatically ordered by date and type, creating a visual timeline of one’s health. Identifying trends, comparing values over time, or preparing a summary for a visit becomes immediate.
Controlled Sharing and Active Privacy
Privacy is not just protection from risks, but the ability to actively decide what to share and with whom:
-
Granular sharing: Ippocra offers a unique way to share medical reports between different facilities via temporary links. The patient can create sharing links (IppoLink), bundling one or more medical reports to share with individual specialists, without exposing the entire documentation. The cardiologist receives only cardiovascular exams, the endocrinologist only endocrine ones.
-
Temporal control: IppoLinks have an automatic expiration, ensuring that access to health data is limited to the strictly necessary period.
-
Full traceability: Every access to shared documentation is logged, allowing the patient to know exactly who viewed what and when.
This level of control transforms the patient from a passive subject of a bureaucratic system into the effective owner of their health information.
Family Management: Beyond the Single Patient
A structural limitation of the EHR is its individual nature: each citizen can access only their own record. While understandable from an institutional privacy standpoint, it ignores a fundamental reality: health is often managed at the family level.
A personal management platform like Ippocra enables the creation of family plans that radically change the paradigm of health organization:
-
Parental coordination: Parents can centrally manage the medical reports of all children, monitoring pediatric visits and development over time, without needing separate system accesses or fragmented documentation.
-
Elderly care: Those caring for older parents can organize their health documentation, coordinate specialist visits, and share clinical information with doctors and caregivers, ensuring continuity of care even remotely.
-
Family overview: A parent can glance at the status of children’s reports, schedule periodic checks, and maintain a complete health chronology for the household, something not always available through the EHR.
This multi‑user management capability is not a technical detail—it answers a concrete need: health is not solely an individual affair; it often involves family dynamics that require adequate coordination and control tools.
Summary: Complementarity, Not Replacement
The Electronic Health Record remains an important tool for institutional interoperability and access to public services. But relying exclusively on it means accepting gaps, fragmentation, and lack of control.
Personal management of medical reports through dedicated platforms does not replace the EHR: it complements, integrates, and places it within a truly patient‑centered health ecosystem.
When Guglielmo started using Ippocra, he didn’t abandon the EHR. He simply stopped depending on it exclusively. Now he is certain that every medical report, regardless of source, is archived, accessible, and shareable according to his needs. The peace of mind that comes from this control is, in itself, a therapeutic benefit.
The question is no longer “EHR or private management?” but “How can I integrate both to achieve complete control of my health?”
Frequently Asked Questions
Will the EHR be replaced by private systems like Ippocra?
No, and it wouldn’t even be desirable. The Electronic Health Record performs important institutional functions and represents a public infrastructure for accessing care. Personal management systems, such as Ippocra, are not substitutes but complements: they fill the EHR’s gaps and give patients active control over their documentation. The optimal approach is the integration of both.
How does data privacy work on a private platform?
Personal medical‑report management platforms operate in compliance with GDPR and Italian/EU health regulations. Data are end‑to‑end encrypted, stored on certified servers, and, most importantly, belong exclusively to the user. Unlike public systems, where data governance involves multiple entities, in a private system the patient is the sole owner and controller. The platform acts as a technical custodian, not the data holder.
Can I automatically import medical reports from the EHR to Ippocra?
Currently, interoperability between the EHR and private platforms is limited by differing regional implementations and the lack of standardized APIs. However, Ippocra allows manual acquisition of medical reports downloaded from the EHR via PDF upload or scanning of paper documents. Ippocra’s technology automatically processes the content, extracting relevant clinical data. It is a hybrid process that requires an initial user action but ensures fully automated management thereafter.
Can I manage the whole family’s medical reports with Ippocra?
Yes, and this is a fundamental difference compared to the EHR. While the Electronic Health Record allows access only to one’s own personal data, Ippocra enables the creation of family plans that include partners, children, and elderly parents. A parent can centrally manage children’s vaccinations, coordinate specialist visits for a dependent elder, and maintain an overall view of family health. This functionality meets a real need: health management often involves the entire family unit, not just the individual.




